Cofactor AI is revolutionizing the way hospitals handle insurance denials and revenue recovery. By harnessing the power of AI, it simplifies and streamlines the complex appeals process, which is often a costly and time-consuming endeavor for healthcare institutions.
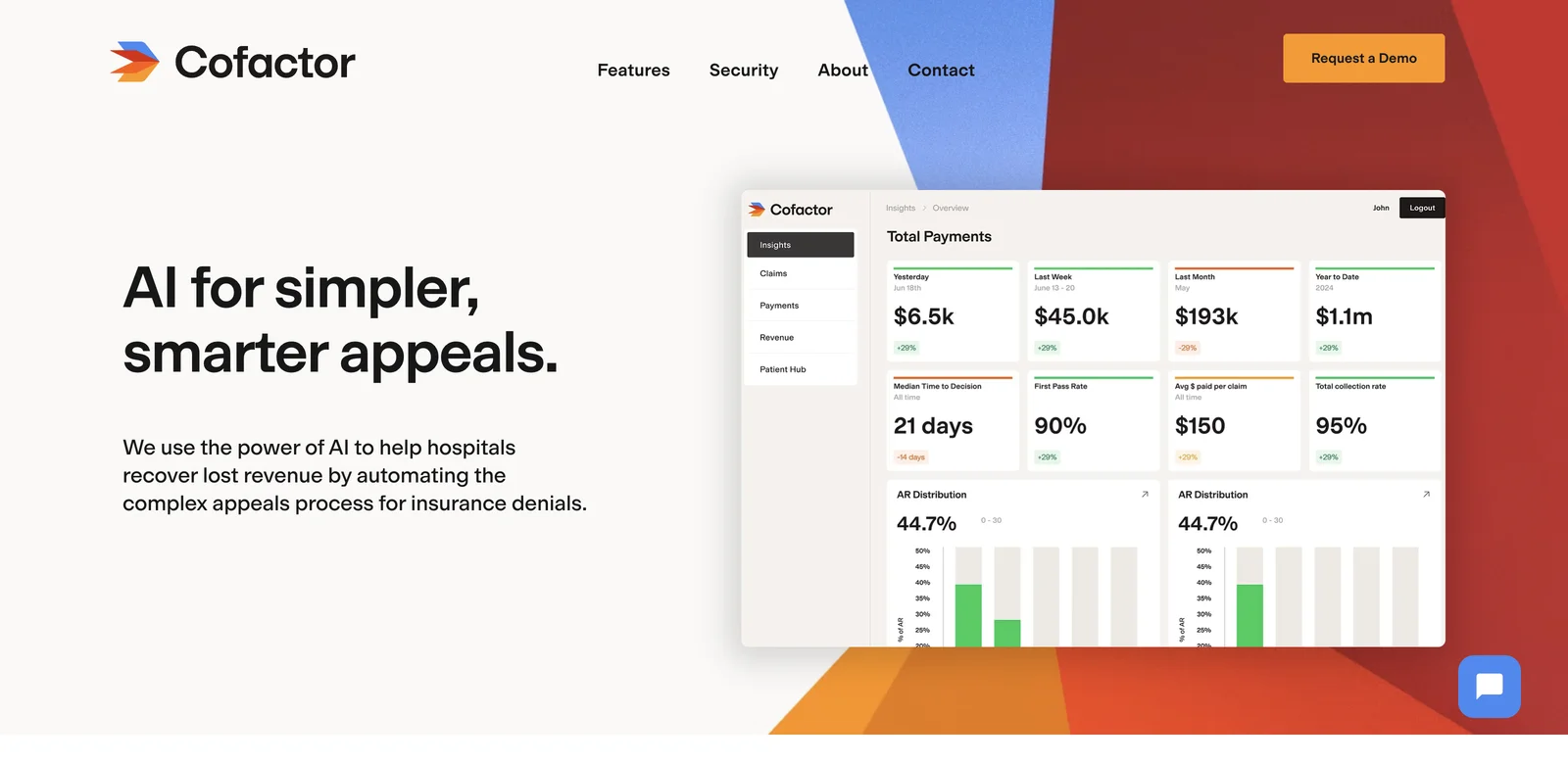
One of the key features of Cofactor AI is its ability to increase overturn rates. It leverages AI-powered insights that are built on millions of data points to accurately identify what evidence payers need. This enables hospitals to win more appeals and transform denied claims into approved reimbursements, thereby maximizing revenue lift.
The platform also significantly improves appeal efficiency. It automates documentation gathering, submission formatting, and status tracking across all payers. This means that the appeals process can be completed much faster, allowing the hospital staff to focus on other high-value activities rather than getting bogged down in administrative tasks.
Another advantage is that Cofactor AI helps recover more revenue per year. Its AI capabilities catch every appealable denial and maximize success rates, effectively transforming denied claims into recovered revenue at scale.
Moreover, it reduces the cost to collect by transforming the costly appeals process into a streamlined, automated workflow. This not only saves money but also frees up the team to concentrate on more important aspects of their work.
In addition, Cofactor AI reduces days outstanding by automating appeals and shortening the time in accounts receivable from months to weeks. This has a positive impact on the hospital's cash flow and overall financial health.
The security of the platform is also a top priority. Cofactor AI has a dedicated compliance team that ensures the highest standards of data security through regular audits and security reviews. They also stay ahead of evolving regulations to protect the sensitive healthcare data of their clients.
Overall, Cofactor AI is a powerful tool that offers numerous benefits to hospitals in terms of revenue recovery, efficiency improvement, and data security.